- Correspondence
- Open access
- Published:
Generation of sarconoids from angiosarcoma patients as a systematic-based rational approach to treatment
Journal of Hematology & Oncology volume 17, Article number: 35 (2024)
Abstract
Angiosarcoma is a rare subtype of malignant neoplasm originating from vascular or lymphatic endothelial cells; its low incidence has posed significant challenges for comprehensive investigations into its pathogenic mechanisms and the development of innovative treatment modalities through in vitro and in vivo models. Recent endeavors spearheaded by patient-partnered research initiatives have aimed to elucidate the intricacies of angiosarcomas by leveraging biological omics approaches, with the overarching objective of enhancing prognostic indicators and therapeutic options for this uncommon pathology. To bridge the gap between preclinical research and translational applications, we engineered angiosarcoma-derived organoids from surgically resected primary tumors, hereafter referred to as “sarconoids,” as a proof-of-concept model. A novel protocol for the establishment of these sarconoids has been developed and validated. To ensure that the sarconoids faithfully recapitulate the heterogeneity and complexities of the patients’ original tumors, including transcriptomic signatures, cell-type specificity, and morphological traits, exhaustive histological and transcriptomic analyses were conducted. Subsequently, we expanded the scope of our study to include an evaluation of a sarconoid-based drug screening platform; for this purpose, a drug library (AOD IX), supplied by the National Cancer Institute’s Developmental Therapeutics Program, was screened using 96-well plates. Our findings suggest that sarconoids can be reliably generated from angiosarcoma patient-derived tissues and can serve as accurate models for evaluating therapeutic responses, thereby holding far-reaching implications for translational research and clinical applications aimed at advancing our understanding and treatment of angiosarcoma.
To the editor
Patient-derived cancer organoids have become increasingly pivotal in pre-clinical and translational cancer research, having been generated from a diverse array of human cancer tissues [1, 2]. Notably, most extant human cancer organoid models are derived from ectodermal or endodermal epithelial progenitors, and, to our knowledge, none have originated from mesenchymal or endothelial tissues [3, 4].
Angiosarcoma is a rare yet aggressive mesenchymal tumor of endothelial origin [5]. There are several specific challenges associated with the clinical development of therapeutics for this disease, such as absence of prior clinical studies, and a lack of information on disease mechanisms and progression [6, 7].
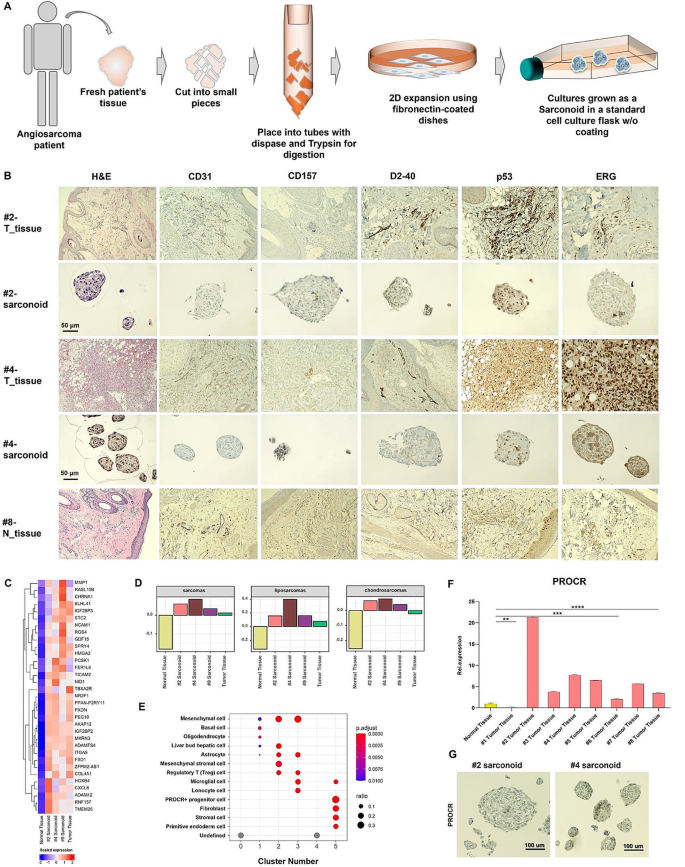
In this study, we propose a methodology to develop personalized angiosarcoma organoid models, termed “sarconoids,” for biological characterization and high-throughput drug screenings. To identify FDA-approved drugs amenable to repurposing for individualized treatment of rare diseases, we generated sarconoids using surgically resected angiosarcoma specimens (Fig. 1a, Fig. S1a). Immunohistochemical analyses and quantitative real-time PCR (qPCR) analyses revealed elevated expression levels of various vascular and mesenchymal markers in both primary tumors and tumor-derived sarconoids, as compared to normal tissues (Fig. 1b, Fig. S1c, Fig S2a-c). To evaluate the angiogenic potential of our sarconoids, we conducted Matrigel-based sprouting assays. The results indicated that they exhibited more extensive matrix sprouting compared to HUVEC spheroids (Fig. S1b, Fig. S2d, e).
Establishment and characterization of sarconoids derived from angiosarcoma patients. (a) Schematic illustration of the workflow for the generation of sarconoids. (b) Histopathological staining of vascular neoplasm markers (CD31, CD157, ERG, and p53) and a lymphatic marker (D2-40) in primary resected angiosarcoma tumors and their corresponding sarconoids; scale bars, 50 μm. (c) Heat map of the scaled FPKM values of representative gene sets significantly upregulated in the patient-derived sarconoids and tumor tissue. (d) Gene set variation analysis (GSVA)-based subtyping of normal tissue, patient #2 tumor tissue, and patient #2-, #4 and #9-sarconoids against published gene sets (GeneRIF Biological Term Annotations), among the sarcoma subtypes. (e) Dot plot of the mean expression of canonical marker genes using the CellMarker database for 14 major lineages from each patient #2-sarconoid cluster, as indicated. (f) Quantification of PROCR expression by qRT-PCR in normal and cancer tissues (n = 3). An unpaired t-test was used; *p < 0.05, **p < 0.01,***p < 0.001,****p < 0.0001. (g) IHC assays of serial sections from patient #2- and patient #4-sarconoids for PROCR expression. Scale bars, 100 μm
To further elucidate the gene expression signature of sarconoids in comparison to their tissues of origin, angiosarcoma tissues and patient-derived sarconoids, collected from consenting patients, were analyzed using RNA-seq (Fig. S3a). A heatmap depicting 33 genes that are upregulated across all four samples is presented in Fig. 1c and Fig. S3e (fold change > 4 and Bonferroni-corrected p < 0.001). Furthermore, gene set enrichment analysis techniques, such as gene set variation analysis, were employed to stratify sarcoma into distinct subgroups based on previously reported data [8]. Patient-derived sarconoids were classified into sarcoma, liposarcoma, and chondrosarcoma categories (Fig. 1d). Hierarchical clustering results revealed an enrichment of angiogenesis-associated genes in both tissue and sarconoids derived from angiosarcomas (Fig. S3f). Gene Ontology (GO) term enrichment analysis of the upregulated differentially expressed genes (DEGs) indicated that a variety of DEGs were enriched in biological processes pertinent to angiogenesis, muscle cell differentiation, and extracellular matrix (ECM) organization (Fig. S3b-d). Conversely, GO terms associated with skin development were overrepresented in the downregulated genes (Fig. S3g).
Utilizing UMAP to embed and cluster our single-cell expression data, we identified six distinct cell populations, labeled C0-C5 (Fig. S4a). Each cluster was mapped to compare its most representative expressed genes with known markers (Fig. S4b-d). Utilizing the CellMarker Database, we were able to assign multiple cell type labels to each cluster (Fig. 1e). Notably, Cluster 5, which partially consists of PROCR-expressing progenitor cells, has been associated with vascular endothelial stem cells [9, 10]. PROCR expression in tissue samples was analyzed using both qRT-PCR and immunohistochemistry, revealing high levels in 8 of the 9 angiosarcoma cases as compared to normal tissue (Fig. 1f and Fig. S5b). Additionally, we performed qRT-PCR analyses to assess PROCR expression in patient-derived sarconoids, finding it to be significantly higher in sarconoids from patients #2 and #4 compared to normal cells (Fig. 1g and Fig. S5a).
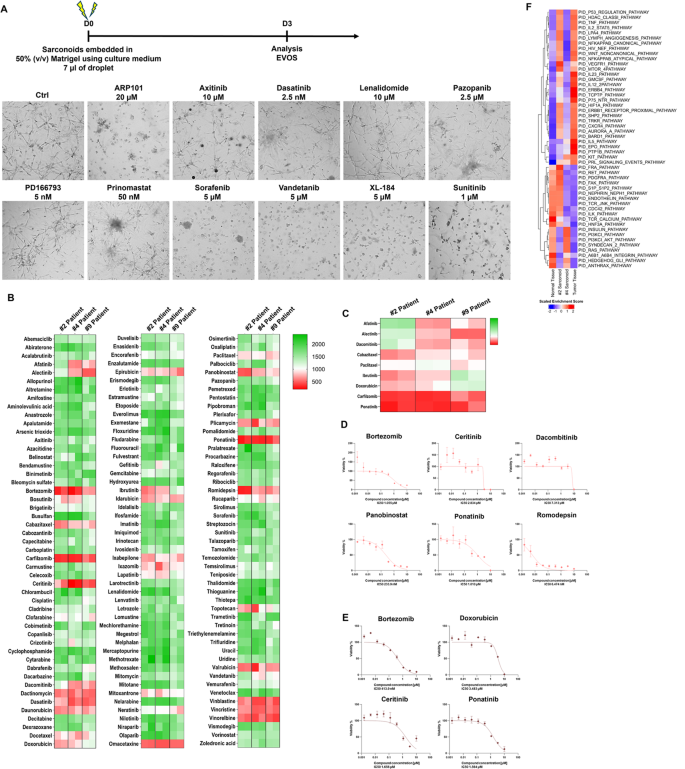
To confirm the suitability of our sarconoid model for drug screening and response prediction, we conducted single-dose trials between 2.5 nM and 20 µM using anti-angiogenic agents on sarconoids derived from patient #4 (Fig. 2a). Using a high-throughput in vitro drug screen, we assessed the cytotoxic activities of 147 FDA-approved compounds on patient-derived sarconoids, observing differing sensitivities between the three sarconoid strains (Fig. 2b). Image-based phenotypic analyses helped categorize individual sarconoids as either insensitive or sensitive to specific treatments (Fig. S6a, b). Overall, 10 compounds demonstrated activity against at least one sarconoid strain. To validate these findings, we performed more comprehensive dose-response assays on 7 active compounds (Fig. 2d, e). Intriguingly, EGFR-TKIs like afatinib and dacomitinib did not significantly impact the viability of sarconoids from patient #2 in our image-based assays, suggesting specific molecular targets and pathways are at play (Fig. 2c). Moreover, sarconoids from patient #2 showed greater sensitivity to histone deacetylase (HDAC) inhibitors like romidepsin and panobinostat (Fig. S6c), suggesting up-regulation of the HDAC pathway in this case (Fig. 2f). Each sarconoid line exhibited unique phenotypic and genomic features, resulting in varied drug sensitivities.
Visualization of high-throughput screening results for 147 FDA-approved compounds against patient-derived sarconoids. (a) Experimental design. Representative bright field images show the morphology of the patient #4-sarconoids after three days of treatment with the indicated compounds at different concentrations. (b) The 147 FDA-approved compounds were tested in patient #2-, #4- and #9-sarconoids. The percentiles for the obtained anti-proliferative values are depicted using a heat map. Low values (indicating resistance) are depicted in green, and high values (indicating sensitivity) in red. Compounds are ordered alphabetically. (c) Heat map of drug effects demonstrating heterogeneous drug responses between the patient #2-, #4-and #9-sarconoids. The columns indicate samples, and the rows indicate the tested drugs and nominal targets. (d) Representative drug response curves for bortezomib, ceritinib, dacombitinib, panobinostat, ponatinib, and romidepsin in patient #2-sarconoid. (e) Representative drug response curves for bortezomib, doxorubicin, ceritinib, and ponatinib in the patient #4-sarconoids. Normalized mean ± SEM (n = 3) viability data from triplicate wells for each drug concentration are presented. (f) Sibling cultures from patients #2 and #4 display heterogeneous pathway activity. The HDAC pathway was specifically activated in only the patient #2-sarconoid tissue, which resulted in a better response to HDAC inhibitor compared to patient #4-sarconoids. Only patient #4-sarconoids showed an upregulation of the PI3K/Akt and RAS pathway, which underpinned their better response to the TKIs. The indicated color code represents scaled mRNA expression across the samples
Each sarconoid line exhibited unique phenotypic and genomic features, resulting in varied drug sensitivities. This underscores the importance of tailoring treatments to individual patients, which may help narrow down therapeutic options and optimize the treatment regimen for angiosarcoma.
Data availability
Any additional information required to reanalyze the data reported in this paper is available from the corresponding authors on reasonable request, gsjeong@amc.seoul.kr.
Abbreviations
- FDA:
-
Food and drug administration
- qPCR:
-
Quantitative real-time PCR
- HUVEC:
-
Human umbilical vein endothelial cells
- RNA-seq:
-
RNA Sequencing
- GO:
-
Gene ontology
- DEGs:
-
Differentially expressed genes
- ECM:
-
Extracellular matrix
- UMAP:
-
Uniform manifold approximation and projection
- PROCR:
-
Protein C receptor
- EGFR:
-
Epidermal growth factor receptor
- TKIs:
-
Tyrosine kinase inhibitors
- HDAC:
-
Histone deacetylases
- HTS:
-
High-throughput screening
References
Vlachogiannis G, Hedayat S, Vatsiou A, Jamin Y, Fernandez-Mateos J, Khan K, Lampis A, Eason K, Huntingford I, Burke R, et al. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science. 2018;359(6378):920–6.
Broutier L, Mastrogiovanni G, Verstegen MM, Francies HE, Gavarro LM, Bradshaw CR, Allen GE, Arnes-Benito R, Sidorova O, Gaspersz MP, et al. Human primary liver cancer-derived organoid cultures for disease modeling and drug screening. Nat Med. 2017;23(12):1424–35.
Eiraku M, Takata N, Ishibashi H, Kawada M, Sakakura E, Okuda S, Sekiguchi K, Adachi T, Sasai Y. Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature. 2011;472(7341):51–6.
Takebe T, Wells JM. Organoids by design. Science. 2019;364(6444):956–9.
Zhang J, Gong H, Wang Y, Zhang G, Hou P. Angiosarcoma of the visceral organs: a morphological, immunohistochemical, and C-MYC status analysis. Pathol Res Pract. 2022;238:154118.
Painter CA, Jain E, Tomson BN, Dunphy M, Stoddard RE, Thomas BS, Damon AL, Shah S, Kim D, Gomez Tejeda Zanudo J, et al. The Angiosarcoma Project: enabling genomic and clinical discoveries in a rare cancer through patient-partnered research. Nat Med. 2020;26(2):181–7.
Weidema ME, Versleijen-Jonkers YMH, Flucke UE, Desar IME, van der Graaf WTA. Targeting angiosarcomas of the soft tissues: a challenging effort in a heterogeneous and rare disease. Crit Rev Oncol Hematol. 2019;138:120–31.
Burns J, Wilding CP, Krasny L, Zhu X, Chadha M, Tam YB, Ps H, Mahalingam AH, Lee ATJ, Arthur A, et al. The proteomic landscape of soft tissue sarcomas. Nat Commun. 2023;14(1):3834.
Yu QC, Song W, Wang D, Zeng YA. Identification of blood vascular endothelial stem cells by the expression of protein C receptor. Cell Res. 2016;26(10):1079–98.
Gur-Cohen S, Lapidot T. Vascular procr(+) stem cells: finding new branches while looking for the roots. Cell Res. 2016;26(10):1071–2.
Acknowledgements
We thank the study patients for agreeing to participate, as well as the study teams at Asan Medical Center, the High Throughput Screening (HTS) Core Lab, for their support with the drug screening analyses. We further thank the NCI Development Therapeutics Program (DTP) for providing the agents used in this study.
Funding
This work was supported by a National Research Foundation of Korea (NRF) (NRF-2022R1F1A1069608), and by the Ministry of Health & Welfare (HR21C0198), and by the Asan Institute for Life Sciences, Asan Medical Center (2021IP0026).
Author information
Authors and Affiliations
Contributions
D.J.J., G.S.J., and J.W.C. designed the study. D.J.J., J.H.B., Y.C.K., and W.S.J. contributed to data gathering and data analysis. D.J.J., J.H.B., Y.C.K., W.S.J., G.S.J., and J.W.C. interpreted the data. D.J.J., J.H.B., Y.C.K., and G.S.J. drafted the manuscript. All authors critically reviewed the manuscript and agreed to its submission for publication.
Corresponding authors
Ethics declarations
Ethical approval
for the study was granted by the Institutional Review Board of Asan Medical Center. Written informed consent was secured from all participating patients.
Conflict of interest
The authors declare no competing financial or other interests in relation to this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jung, D.J., Byeon, J.H., Kim, Y.C. et al. Generation of sarconoids from angiosarcoma patients as a systematic-based rational approach to treatment. J Hematol Oncol 17, 35 (2024). https://doi.org/10.1186/s13045-024-01556-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13045-024-01556-3